Insulin Resistance: The Hidden Metabolic Driver of Ageing
A simple guide to the metabolic slowdown behind fatigue, inflammation, cravings — and accelerated ageing.
This article is part of the Biology of Ageing hub, where we explain the core mechanisms that drive ageing — and how everyday habits influence them over time.
Disclaimer: This article is for educational purposes only and does not replace medical advice. If you have diabetes, prediabetes, PCOS, fatty liver disease, or you use glucose-lowering medication (including insulin), speak with a qualified healthcare professional before making major diet, fasting, or exercise changes.
Insulin resistance is one of the most important — and most overlooked — drivers of accelerated ageing. It quietly affects energy levels, weight regulation, inflammation, blood sugar control, hormone balance, and long-term disease risk.
The encouraging part is that insulin resistance is also highly reversible. Small, consistent habits can meaningfully improve insulin sensitivity at almost any age.
Personal note: I used to think “blood sugar stuff” only mattered if you had diabetes. Then I noticed how much my energy, cravings, and sleep quality changed just by walking after meals and tightening up late-night snacking. It wasn’t dramatic — it was simply consistent.
In this guide, you’ll learn:
- what insulin resistance actually is (in plain English)
- how it develops gradually over time
- why it accelerates ageing and inflammation
- the simplest habits that improve insulin sensitivity naturally
If you want the “big picture” first, start here: Why Longevity Matters and Metabolic Flexibility.
The Simple Explanation
Insulin is a hormone that helps move glucose (sugar) from your bloodstream into your cells, where it’s used for energy.
When cells respond well to insulin, blood sugar stays stable and energy feels consistent. However, when cells stop responding properly — a state called insulin resistance — your body must produce more and more insulin to get the same effect.
This tends to lead to:
- higher blood sugar (especially after meals)
- chronically elevated insulin
- weight gain (often around the midsection)
- lower, more unstable energy
- higher background inflammation
Longevity angle: insulin resistance pushes your body toward “storage mode” instead of “repair mode.” Over time, that shift speeds up many processes linked to ageing.
The Science Explained Simply
Insulin’s job: escort glucose into cells.
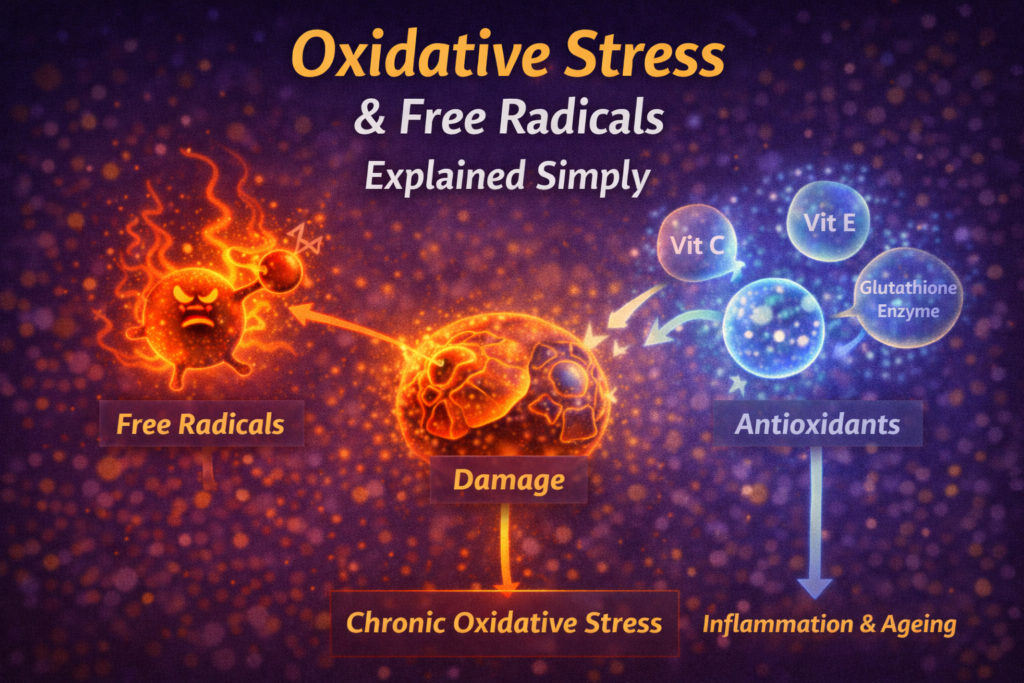
What goes wrong: cells become less responsive to insulin due to repeated energy overload, inactivity, inflammation, poor sleep, chronic stress, and highly processed diets.
The body compensates: by producing more insulin to keep blood sugar under control. For a while, blood sugar can look “normal” — but insulin is working overtime behind the scenes.
Chronically high insulin can drive:
- increased fat storage
- higher inflammatory signalling
- disrupted appetite and cravings
- stiffer blood vessels over time
- reduced metabolic flexibility
Over time, insulin resistance increases the risk of type 2 diabetes, heart disease, fatty liver disease and cognitive decline.
From a biology-of-ageing perspective, insulin resistance interacts with multiple hallmarks — particularly inflammation, mitochondrial dysfunction, and cellular senescence. (Related: Mitochondria & Ageing and Cellular Senescence Explained.)
A useful high-level overview can be found here: Insulin resistance and metabolic disease (NCBI) .
The Metabolic Spiral
Insulin resistance typically develops through a predictable cycle:
- Frequent intake of highly processed / high-sugar foods → rapid glucose spikes
- Rising insulin to control blood sugar
- Cells become less responsive due to constant exposure
- Insulin rises further to compensate
- Fatigue, cravings and weight gain increase
- Inflammation rises → ageing accelerates
The key insight: you don’t need to break the entire cycle at once. Interrupting just a few steps consistently is often enough to reverse the trend.
How This Shows Up Day-to-Day
Insulin resistance isn’t just a lab concept — it has a “feel” in real life. Common patterns include:
- energy dips 1–3 hours after carb-heavy meals
- strong cravings for sweet snacks in the afternoon or evening
- sleep disruption (especially with late eating or alcohol)
- stubborn belly fat despite “not eating that much”
- brain fog and low drive on sedentary weeks
None of these “prove” insulin resistance on their own. However, they’re often early hints that your metabolism would benefit from the habits in the next section.
How to Improve Insulin Sensitivity Naturally
A) Move After Meals (highest ROI habit)
One of the fastest and most reliable ways to improve insulin sensitivity is simple movement after eating. It helps muscles absorb glucose with less insulin.
- 5–10 minute walk after meals
- light stretching or mobility after dinner
- standing or gentle activity instead of sitting immediately
See: Why Walking After Meals Extends Lifespan
B) Strength Training (build the “glucose sink”)
Muscle is one of the largest glucose sinks in the body. More (and better functioning) muscle means better glucose disposal and lower insulin demand.
- 2–3 full-body sessions per week
- compound patterns (squat, hinge, push, pull, carry)
- train at a controlled, challenging effort — not reckless intensity
See: Strength Training for Longevity
C) Zone 2 Cardio (mitochondria + flexibility)
Low-to-moderate intensity cardio supports mitochondrial health and improves metabolic flexibility — meaning you can switch between burning carbs and fat more effectively.
- 2–3 sessions per week
- conversational pace
See: Zone 2 Cardio
D) Eat to Reduce Glucose Spikes (without going extreme)
- pair carbohydrates with protein and fat
- start meals with fibre/veg when possible
- choose slower-release carbs (oats, lentils, beans, whole grains)
- minimise ultra-processed foods and sugary drinks
This pairs naturally with: Blood Sugar & Longevity and Anti-Inflammatory Foods.
E) Improve Sleep (insulin sensitivity is fragile)
Even one poor night of sleep can reduce insulin sensitivity the next day. In other words, sleep debt often shows up as cravings and “easy weight gain.”
- consistent sleep and wake times
- cool, dark sleeping environment
- limit screens late at night
See: Sleep for Longevity
F) Reduce Chronic Stress (cortisol affects glucose)
Elevated cortisol makes cells less responsive to insulin. Reducing baseline stress improves metabolic health indirectly but powerfully.
- daily walking
- short breathwork sessions
- stable routines and realistic training volume
See: Breathwork That Lowers Cortisol Fast and Stress & Longevity.
Quick Wins
- walk after your largest meal
- add protein to your first meal
- swap sugary snacks for yoghurt, nuts, or fruit
- add one weekly strength session
- get outside for morning light (helps your daily metabolic rhythm)
- increase sleep by 15–30 minutes
What Not to Do
- don’t cut out all carbs — pairing and timing usually matter more than extremes
- don’t rely on supplements to “fix” insulin resistance
- don’t ignore sleep — it’s foundational
- don’t overtrain while under-recovering
- don’t snack constantly — it keeps insulin elevated
A Simple Insulin-Friendly Weekly Plan
- Most days: 5–10 minute walk after at least one meal
- 2–3× per week: strength training
- 2× per week: Zone 2 cardio
- Daily default: protein + fibre at meals
- Nightly: consistent wind-down + 7–9 hour sleep window
For most people, this combination leads to noticeable improvements in energy, appetite control, and metabolic stability within weeks — because it targets the biggest levers repeatedly.
FAQs
Can insulin resistance be reversed?
Often, yes. Many people see improvements within weeks of consistent habits. Deeper change typically takes longer — but it’s absolutely possible.
Do I need a glucose monitor?
Helpful for feedback, but not essential. Energy stability, cravings, waist measurement, and fasting glucose/HbA1c (via your clinician) can also guide progress.
Does fasting help?
A simple 12–14 hour overnight fasting window can help many people. If you’re on medication, do this with medical guidance.
Is weight loss required?
Not always. Muscle gain, better sleep, and movement can improve insulin sensitivity even without major weight change.
UK Specific Notes
- low-cost staples: oats, lentils, beans, frozen veg, eggs, Greek yoghurt, tinned fish
- home workouts support consistency during dark/wet months
- morning daylight exposure matters more in UK winter (even grey light helps)
- budget-friendly snacks: apples, nuts, yoghurt, carrots + hummus
- if you’re concerned, ask your GP about HbA1c, fasting glucose, and triglycerides/HDL as practical markers
If You Take One Thing From This
Insulin resistance accelerates ageing — but it’s also one of the most reversible metabolic problems. Post-meal movement, strength training, better sleep, and balanced meals can shift the trajectory fast.
Want a simple, repeatable metabolic routine?
Use this as your default: morning light, a protein-first meal, and a short walk after meals. If you want it laid out as a daily structure, the checklist makes it effortless.
Related Articles
- Why Longevity Matters
- Metabolic Flexibility
- Blood Sugar & Longevity
- Why Walking After Meals Extends Lifespan
- Strength Training for Longevity
- Zone 2 Cardio
- Sleep for Longevity
- Stress & Longevity
References
- DeFronzo RA, Ferrannini E. Insulin resistance: a multifaceted syndrome. Diabetes Care.
- NCBI. Insulin resistance and metabolic disease. View source
Disclaimer: This content is for educational purposes only and does not replace medical advice. If you have diabetes, prediabetes, eating disorder history, or are using glucose-lowering medications, consult a qualified healthcare professional before changing diet, fasting, or exercise routines.
— Simon
Longevity Simplified
Simon is the creator of Longevity Simplified, where he breaks down complex science into simple, practical habits anyone can follow. He focuses on evidence-based approaches to movement, sleep, stress and nutrition to help people improve their healthspan.