Why Poor Sleep Makes Stress Worse (and Vice Versa)
Sleep and stress form a feedback loop. When one breaks down, the other quietly follows — accelerating fatigue, anxiety and biological ageing.
Disclaimer: This article is for educational purposes only and does not provide medical advice. Persistent insomnia, sleep apnoea symptoms, severe anxiety, depression or unexplained fatigue should be assessed by a qualified clinician.
Most people treat sleep and stress as separate problems. You either “fix your sleep” or “manage your stress”.
In reality, they’re tightly linked in a two-way feedback loop. Poor sleep increases stress sensitivity, emotional reactivity and cortisol disruption. Elevated stress then fragments sleep even further — making recovery progressively harder.
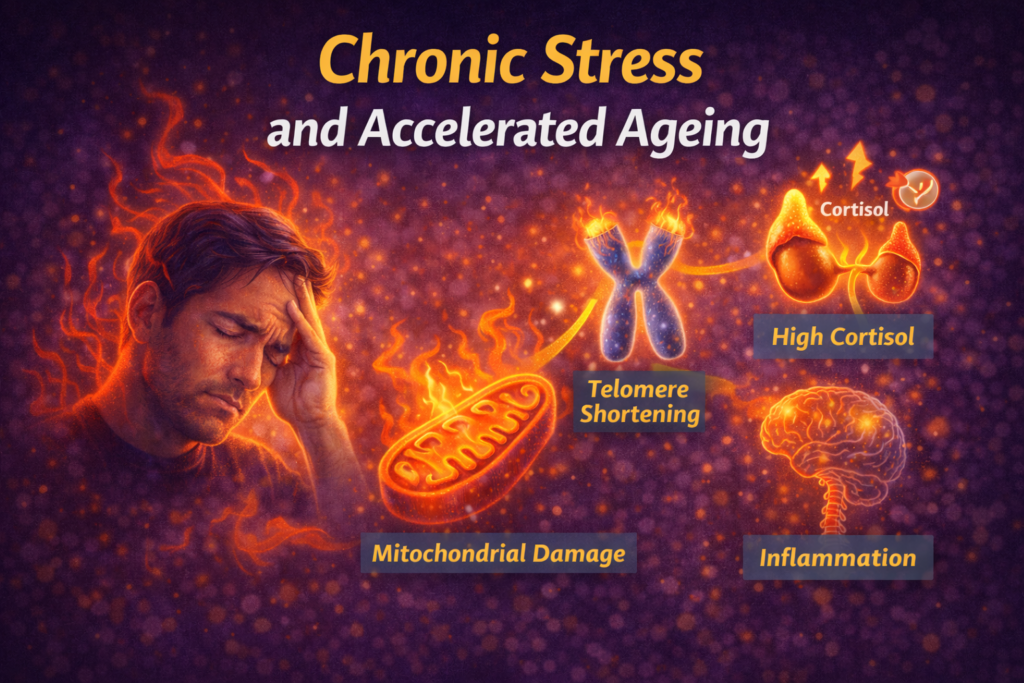
Over time, this loop quietly accelerates fatigue, inflammation, metabolic instability and biological ageing. The good news: breaking even one side of the loop produces compounding benefits.
Personal observation: When my sleep slips, everything feels harder — patience drops, cravings rise, and small stressors feel bigger than they should. Fixing sleep almost always stabilises stress faster than trying to “think my way” into calm.
1) The sleep–stress loop explained simply
Think of sleep and stress as a seesaw:
- good sleep → better emotional regulation, lower baseline stress
- poor sleep → higher stress sensitivity and nervous system reactivity
- high stress → lighter, more fragmented sleep
- fragmented sleep → even higher stress the next day
Once this loop establishes, people often chase symptoms — caffeine for fatigue, willpower for anxiety, supplements for sleep — without addressing the reinforcing cycle underneath.
This loop connects directly into: Stress and Inflammation, Stress and Blood Sugar Instability, and Chronic Stress and Accelerated Ageing.
2) How poor sleep increases stress
Emotional regulation weakens
Sleep loss reduces activity in brain regions responsible for impulse control and emotional regulation. Small problems feel larger. Frustration rises faster. Anxiety thresholds drop.
Cortisol rhythm becomes disrupted
Poor sleep blunts the normal morning cortisol rise and delays evening decline — keeping the nervous system in a semi-alert state.
See: How to Tell if Your Cortisol Rhythm Is Off.
Blood sugar stability worsens
Short sleep reduces insulin sensitivity and increases cravings for fast energy, making emotional and physiological stress harder to regulate.
Related: Stress Appetite.
Pain sensitivity and inflammation increase
Fragmented sleep increases inflammatory signalling and pain sensitivity — which itself becomes a stressor.
3) How stress damages sleep
Hyperarousal delays sleep onset
Elevated sympathetic tone makes it harder to transition into sleep — even when physically tired.
This shows up clearly in: Evening Anxiety.
Sleep becomes lighter and more fragmented
Stress reduces deep sleep and increases micro-awakenings — lowering recovery quality even if total hours look acceptable.
Autonomic recovery slows
Parasympathetic activity (recovery mode) is suppressed under chronic stress, impairing overnight nervous system reset.
See: Vagus Nerve Basics.
4) Signs you’re stuck in the loop
- waking up tired despite adequate time in bed
- feeling emotionally reactive or easily overwhelmed
- difficulty switching off at night
- increased cravings and caffeine dependence
- lower exercise tolerance or slower recovery
- persistent background tension
These patterns often coexist rather than appearing in isolation.
5) How to break the loop (practical steps)
Anchor sleep timing first
Consistency matters more than perfection. Stable wake and bed times strengthen circadian signalling.
Foundations: Sleep for Longevity.
Reduce evening stimulation
- dim lights after sunset
- limit emotionally charged content
- reduce late caffeine
Use daily nervous system downshifts
Small calming inputs compound: The 2-Minute Downshift, Box Breathing vs Physiological Sigh.
Stabilise blood sugar earlier in the day
Protein, fibre, post-meal walks and avoiding long fasts reduce nighttime instability.
See: Stress and Blood Sugar Instability.
Train to support recovery — not overwhelm it
Match intensity to recovery capacity: High vs Low Cortisol Training Days and Movement for Stress & Recovery.
6) Using wearables to spot the pattern
Wearables help reveal the sleep–stress loop through:
- suppressed HRV trends
- elevated resting heart rate
- late sleep onset
- fragmented sleep architecture
Focus on trends rather than daily noise: Wearables & Recovery Tracking and Tracking Trends, Not Daily Noise.
FAQ
Should I fix sleep or stress first?
Start with whichever is easiest to stabilise. Improving either side often helps the other.
Can supplements solve this loop?
Supplements may support symptoms, but behaviour and timing drive the core reset.
How long does it take to break the loop?
Many people notice improvement within 2–4 weeks of consistent changes.
Does this affect ageing?
Yes. Chronic sleep–stress disruption accelerates inflammation, metabolic dysfunction and biological ageing.
Final takeaway
Sleep and stress don’t operate independently — they amplify each other.
Stabilise sleep timing, reduce evening stimulation, build daily downshifts and protect recovery. Break the loop gently and consistently — not aggressively.
— Simon
References
- Walker MP. Why We Sleep — sleep, emotional regulation and stress biology.
- National Sleep Foundation — Sleep and stress relationship overview.
- Spiegel K et al. (2009). Impact of sleep debt on metabolic and endocrine function.
Simon is the creator of Longevity Simplified, where he breaks down complex science into simple, practical habits anyone can follow. He focuses on evidence-based approaches to movement, sleep, stress and nutrition to help people improve their healthspan.