Stress and Inflammation: The Quiet Loop That Accelerates Ageing
Chronic stress doesn’t just affect how you feel — it quietly amplifies inflammation, recovery load and long-term biological wear.
Disclaimer: This article is for educational purposes only and does not provide medical advice. If you have autoimmune disease, chronic inflammatory conditions, persistent pain, or unexplained symptoms, consult a qualified clinician.
Inflammation is often discussed as a nutrition problem — sugar, seed oils, ultra-processed foods. However, one of the most underestimated drivers of chronic inflammation is persistent stress.
Stress doesn’t just make you feel tense. It alters immune signalling, sleep quality, glucose regulation and recovery capacity. Over time, this creates a self-reinforcing loop where stress drives inflammation — and inflammation feeds back into stress sensitivity.
Understanding this loop gives you leverage. It shifts the conversation away from chasing anti-inflammatory hacks and toward stabilising the systems that actually regulate inflammation long-term.
Personal observation: I used to think inflammation was purely a food problem. Once I started tracking how sleep debt, work intensity and psychological load affected my recovery and joint stiffness, the stress–inflammation connection became impossible to ignore.
1) What inflammation actually is
Inflammation is the immune system’s repair and defence response. In the short term, it’s protective — helping fight infection, heal injury and adapt to stress.
Problems arise when inflammation becomes chronically elevated at low levels. This “smouldering” inflammation is associated with cardiovascular disease, insulin resistance, neurodegeneration and accelerated ageing.
Ageing researchers sometimes refer to this pattern as inflammaging — the gradual rise in baseline inflammatory tone with age.
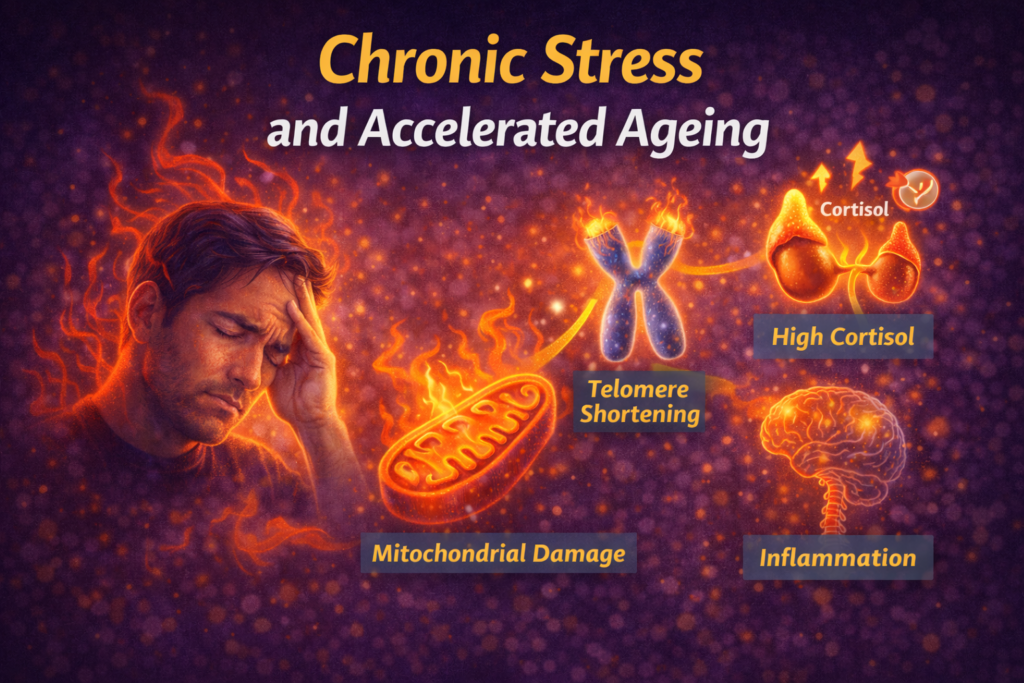
2) How stress increases inflammation
Stress hormones alter immune signalling
Acute stress temporarily suppresses certain immune responses — which is adaptive. Chronic stress, however, dysregulates immune balance and promotes inflammatory signalling.
Sleep fragmentation amplifies inflammatory markers
Poor sleep increases pro-inflammatory cytokines and reduces recovery capacity. Stress-driven sleep disruption compounds this effect.
Related: Sleep for Longevity.
Blood sugar instability fuels inflammatory load
Glucose swings increase oxidative stress and inflammatory signalling. Stress makes glucose regulation less stable.
See: Blood Sugar & Longevity.
Reduced recovery capacity
Chronic sympathetic activation reduces tissue repair efficiency and autonomic recovery — allowing inflammation to persist.
3) The stress–inflammation feedback loop
The loop looks like this:
- psychological or physical stress increases arousal
- sleep quality and metabolic stability decline
- inflammatory signalling rises
- inflammation increases fatigue, pain and stress sensitivity
- baseline stress load rises further
Over time, this loop quietly accelerates biological wear — even in people who appear “healthy” on the surface.
This mechanism underpins much of what’s explored in: Chronic Stress and Accelerated Ageing.
4) Signs your inflammation load may be stress-driven
- persistent low-grade aches or stiffness
- frequent minor illnesses or slow recovery
- brain fog or low-grade fatigue
- poor sleep quality despite adequate time in bed
- heightened stress reactivity
None of these prove inflammation — but together they often indicate recovery strain rather than purely dietary issues.
5) What actually reduces the loop
Stabilise sleep first
Sleep is the strongest anti-inflammatory behaviour most people underutilise.
Lower daily nervous system load
Short downshifts accumulate: The 2-Minute Downshift, Box Breathing vs Physiological Sigh.
Move consistently — not excessively
Moderate movement reduces inflammation; overtraining increases it.
See: High vs Low Cortisol Training Days.
Eat for metabolic stability
Focus on fibre, protein, whole foods and glycaemic stability rather than chasing anti-inflammatory superfoods.
See: Anti-Inflammatory Foods.
Reduce chronic psychological load
Boundaries, recovery, social safety and pacing matter as much as supplements.
6) How wearables reveal recovery strain
While you can’t directly measure inflammation at home, wearables can reveal recovery strain that often correlates with inflammatory load:
- persistently elevated resting heart rate
- suppressed HRV trends
- fragmented sleep
- poor recovery scores
Use trends rather than single readings: Wearables & Recovery Tracking, Tracking Trends, Not Daily Noise, and HRV Explained Simply.
FAQ
Can stress alone cause inflammation?
Chronic stress can meaningfully increase inflammatory signalling even without obvious dietary or disease drivers.
Should I take anti-inflammatory supplements?
Supplements may help specific deficiencies, but behavioural recovery inputs drive the largest effect.
How fast does inflammation improve?
Many markers improve within weeks when sleep and stress stabilise — but consistency matters.
Does inflammation directly affect ageing?
Yes. Chronic inflammation is strongly linked to accelerated biological ageing and disease risk.
Final takeaway
Inflammation isn’t just a food problem — it’s a recovery problem.
When stress remains elevated and recovery stays compromised, inflammation quietly accumulates. Stabilising sleep, nervous system load and metabolic inputs reduces the loop far more reliably than chasing hacks.
— Simon
References
- Furman D et al. (2019). Chronic inflammation in the etiology of disease across the life span. Nature Medicine.
- Cohen S et al. (2012). Chronic stress, glucocorticoid receptor resistance, inflammation, and disease risk. PNAS.
- National Institute on Aging — Inflammation and ageing overview.
Simon is the creator of Longevity Simplified, where he breaks down complex science into simple, practical habits anyone can follow. He focuses on evidence-based approaches to movement, sleep, stress and nutrition to help people improve their healthspan.