Stress and Blood Sugar Instability: Why You Crash (and How to Stabilise Your Energy)
Stress doesn’t just live in your head — it changes glucose regulation. The result is cravings, crashes, irritability and fatigue that feel “random”.
Disclaimer: This article is for educational purposes only and does not provide medical advice. If you have diabetes, reactive hypoglycaemia, unexplained dizziness/fainting, or take glucose-lowering medication, speak with a qualified clinician before changing diet or activity.
If you’ve ever felt calm one moment and irritable the next — or energetic in the morning and wiped out by mid-afternoon — there’s a good chance it wasn’t “just mood”.
Stress changes how your body handles energy. It can raise blood glucose, make insulin response less effective, and push you toward faster carbs for relief. Over time, this creates blood sugar swings that feel like crashes: fatigue, brain fog, cravings, and a shorter fuse.
The good news: you don’t need a perfect diet to stabilise this. You need a few repeatable defaults — and an understanding of how stress and glucose interact.
Personal observation: When my workload is high, I can “feel” blood sugar instability as impatience and hunger that arrives too fast. If I stabilise meals and add a short downshift, the whole day feels easier — even when the schedule doesn’t change.
1) The simple explanation
Stress prepares your body for action. One way it does this is by making more energy available in the bloodstream — glucose. That’s useful in a true emergency.
But modern stress is often psychological and prolonged: deadlines, screens, poor sleep, constant stimulation. So the body keeps mobilising glucose — then you get instability:
- glucose rises too easily
- insulin becomes less effective under stress
- energy feels less stable
- cravings rise
- crashes become more frequent
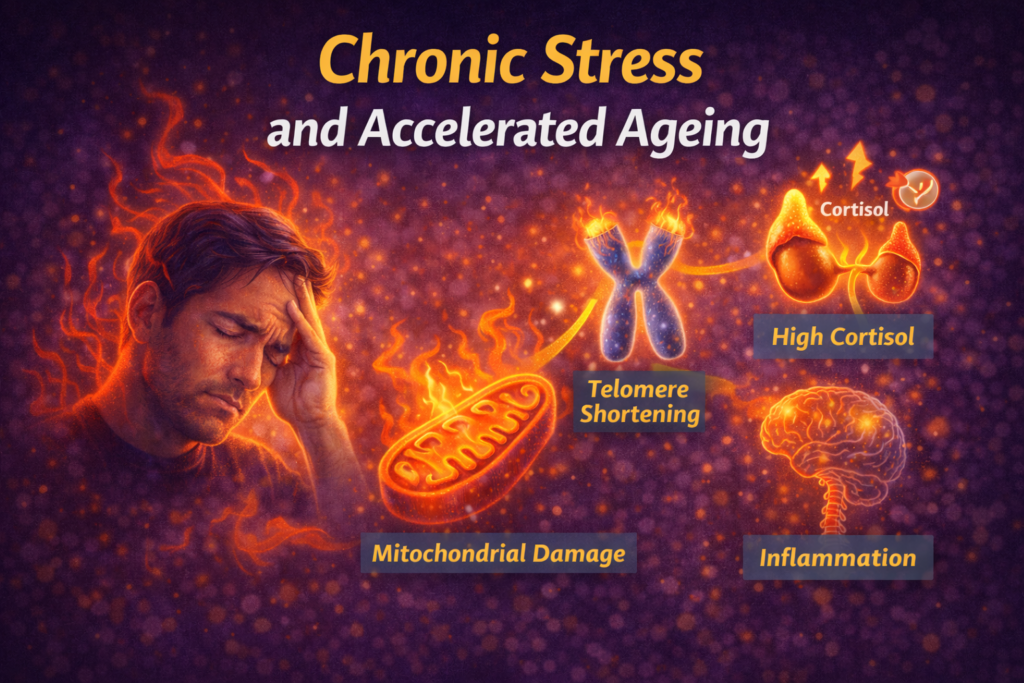
This is one reason stress quietly accelerates ageing and metabolic decline. If you want the bigger picture, start here: Stress and Inflammation and Chronic Stress and Accelerated Ageing.
2) How stress disrupts blood sugar
Stress hormones raise glucose availability
Cortisol and adrenaline help mobilise glucose so you can respond quickly. Under chronic stress, this effect becomes persistent rather than occasional.
If cortisol timing is off, this often shows up as energy dysregulation: How to Tell if Your Cortisol Rhythm Is Off.
Sleep loss makes insulin sensitivity worse
Short or fragmented sleep reduces glucose tolerance and increases appetite for energy-dense food. This makes “normal eating” feel harder and cravings feel louder.
Foundations: Sleep for Longevity.
Stress drives faster food choices
Under stress, the brain prioritises fast reward and fast energy. That usually means refined carbs and sugar. Unfortunately, those foods can amplify swings and worsen the next crash.
Related: Stress Appetite.
3) Why you crash (the common patterns)
Pattern A: High-carb breakfast → late morning crash
A refined-carb breakfast can spike glucose quickly, then drop energy later. Stress amplifies this pattern.
Pattern B: Under-eating → urgent hunger → overeating
Skipping meals seems “productive” until energy collapses. Then cravings arrive with urgency.
Pattern C: Stress + caffeine → jittery energy → afternoon crash
Caffeine can mask fatigue and amplify sympathetic arousal. Later, the rebound can feel like a crash and increase cravings.
Pattern D: Poor sleep → all-day instability
Sleep debt increases hunger and reduces impulse control, making stability harder throughout the day.
Pattern E: Hard training + high stress → depleted recovery
If your stress load is high, intense training can push you into bigger swings — not because exercise is bad, but because recovery is limited. See: High vs Low Cortisol Training Days.
4) Signs your crashes are glucose-related
- irritability or anxiety that improves after eating
- strong cravings for sweet or starchy foods
- energy dips 1–3 hours after meals
- brain fog with sudden hunger
- shaky or “wired” feelings when meals are delayed
Again: none of these diagnose blood sugar issues, but they’re common clues that stability is the missing lever.
5) How to stabilise energy (practical steps)
1) Build meals around protein + fibre
Protein and fibre slow glucose rise and improve satiety. It doesn’t need to be complicated:
- eggs + fruit + yoghurt
- Greek yoghurt + berries + nuts
- chicken/tuna + salad + olive oil
- beans/lentils + vegetables
For a deeper framework: Blood Sugar & Longevity.
2) Add a short walk after meals
Even 10 minutes of easy walking after eating can improve glucose handling and reduce the size of spikes. This is one of the simplest interventions with outsized return.
3) Don’t let the day go “too long” without food
If you reliably crash, experiment with a stabilising snack mid-afternoon instead of trying to power through.
4) Use a 2-minute downshift before reaching for sugar
Stress cravings often happen in a state of arousal, not hunger. Run this first: The 2-Minute Downshift.
Then choose a stabilising option (protein + fibre) if you’re genuinely hungry.
5) Protect sleep timing
Sleep is the foundation for stable appetite and glucose regulation. If your evenings are wired, read: Evening Anxiety.
6) Training and stress: when workouts worsen crashes
Exercise generally improves insulin sensitivity — but context matters.
If you’re already under-recovered (poor sleep, high stress, low HRV trend), adding high intensity can increase stress hormones and worsen swings temporarily. In that phase, prioritise:
- walking
- mobility
- Zone 2 cardio (gentle)
- strength work with sensible volume
See: Movement for Stress & Recovery.
7) Wearables: how to spot the pattern
Wearables can’t measure glucose directly unless you use a CGM, but they can reveal stress and recovery strain that correlates with instability:
- elevated resting heart rate
- suppressed HRV trends
- fragmented sleep
- late bedtime patterns
Use trends, not single readings: Wearables & Recovery Tracking and Tracking Trends, Not Daily Noise.
FAQ
Is this the same as diabetes?
No. Many people experience glucose instability without diabetes. If symptoms are severe or frequent, get assessed.
Should I cut carbs?
Usually not necessary. The goal is stability: pair carbs with protein, fibre and movement.
Why do I crave sugar most at night?
Night cravings often reflect accumulated stress load, sleep pressure and missed stability earlier in the day. See: Stress Appetite.
Does stress-induced glucose instability affect ageing?
Yes. Chronic glucose swings contribute to inflammation and metabolic decline, which increases ageing-related risk. See: Stress and Inflammation.
Final takeaway
If you crash, crave sugar, and feel emotionally reactive under stress, don’t assume it’s just mindset. Stress changes glucose regulation.
Stabilise sleep, build protein-and-fibre meals, walk after eating, and use short nervous system resets. Small stability inputs compound — and the crashes usually soften.
— Simon
References
- American Diabetes Association — Stress and blood glucose overview. Reference
- CDC — Diabetes and stress (general education on stress effects on glucose). Reference
- Your internal guide: Blood Sugar & Longevity.
Simon is the creator of Longevity Simplified, where he breaks down complex science into simple, practical habits anyone can follow. He focuses on evidence-based approaches to movement, sleep, stress and nutrition to help people improve their healthspan.