Inflammaging Explained: Why Inflammation Rises With Age (and What Actually Helps)
Inflammaging is the slow, chronic rise in baseline inflammation that drives many age-related diseases. It’s not about eliminating inflammation — it’s about restoring regulation, recovery and resilience.
← Back to: Biology of Ageing Explained
Disclaimer: This article is for educational purposes only and does not provide medical advice. It is not intended to diagnose, treat or prevent disease. Always consult a qualified professional before making health or supplement changes.
As we age, many people develop a quiet, persistent elevation in inflammatory signalling — even without obvious illness or injury. This phenomenon is known as inflammaging.
Unlike acute inflammation (which heals injuries and fights infection), inflammaging is low-grade, chronic and often invisible. Yet it strongly predicts cardiovascular disease, metabolic dysfunction, cognitive decline, frailty and overall mortality risk.
Importantly, inflammaging is not one single cause. It emerges from interacting systems: immune ageing, cellular damage accumulation, mitochondrial stress, gut permeability, metabolic instability and nervous system load.
This guide explains what inflammaging actually is, why it rises with age, and how to lower inflammatory load safely without suppressing essential immune function.
Personal observation: Once I started viewing inflammation as a systems problem — not a single biomarker — lifestyle decisions became far more coherent. Sleep, movement, gut health and stress regulation all feed the same inflammatory dial.
1) The simple explanation
Inflammaging means a gradual rise in baseline inflammation as you age.
It’s not dramatic like an infection or injury — instead, it’s a low-level background signal that never fully switches off.
Over years, this chronic inflammatory load accelerates tissue wear, metabolic dysfunction, vascular damage and immune exhaustion.
The goal is not to eliminate inflammation (which would impair healing and immunity), but to restore balance and recovery capacity.
2) What inflammaging actually is
Inflammaging reflects a shift in immune regulation:
- higher baseline inflammatory signalling
- slower resolution of inflammatory responses
- reduced immune precision
- greater tissue sensitivity to stress
Common biomarkers include CRP, IL-6, TNF-α and related cytokines — but the biological effect matters more than any single number.
Related foundation: Stress and Inflammation.
3) Why inflammation rises with age
Several overlapping systems drive inflammaging:
- accumulated cellular damage
- senescent cell signalling
- mitochondrial dysfunction
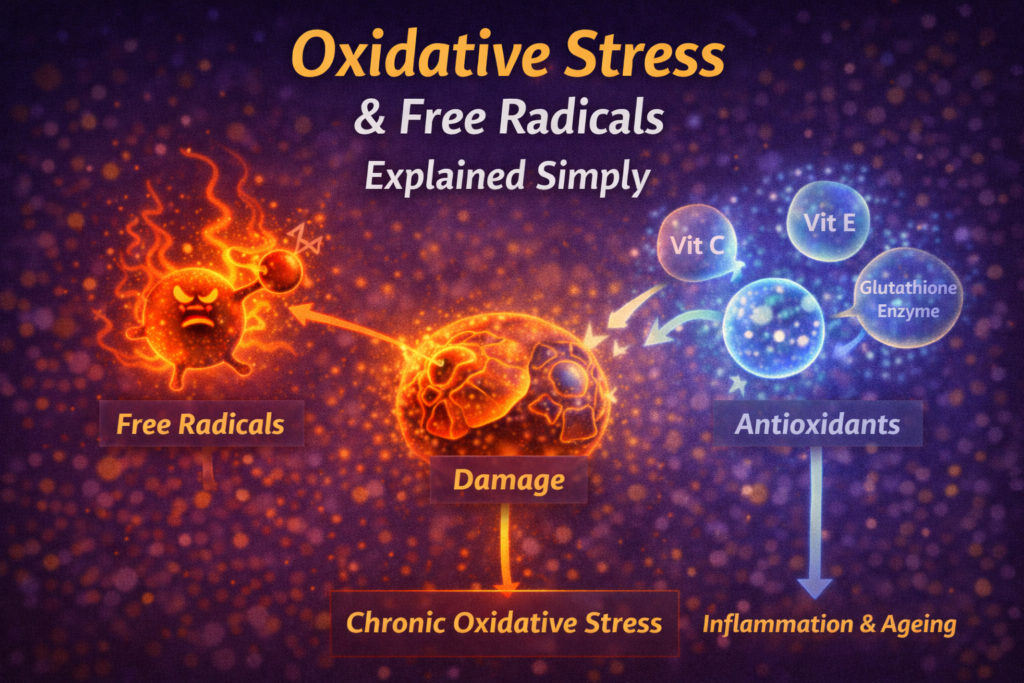
- oxidative stress feedback loops
- immune ageing (immunosenescence)
- metabolic instability
- gut barrier changes
- chronic stress exposure
No single lever explains the whole phenomenon — which is why lifestyle stacks matter more than isolated fixes.
4) Senescent cells and inflammatory signalling
Senescent cells are damaged cells that no longer divide but remain metabolically active. They release inflammatory signals known as the SASP (senescence-associated secretory phenotype).
As senescent cells accumulate, inflammatory signalling rises even without infection or injury.
See: Cellular Senescence Explained.
5) Mitochondria, oxidative stress and immune activation
Damaged mitochondria leak reactive oxygen species and danger signals that activate immune pathways.
Poor mitochondrial quality therefore increases both oxidative stress and inflammatory tone.
Related: Mitochondria & Ageing, Mitophagy Explained and Inflammation vs Oxidative Stress.
6) The gut–immune connection
The gut barrier normally prevents bacterial fragments from entering circulation.
With age, permeability can increase, allowing low-grade immune activation — sometimes called metabolic endotoxemia.
Fibre intake, microbial diversity and polyphenol metabolism strongly influence this pathway.
Related: Polyphenols Explained.
7) Metabolic stress and inflammatory load
Blood sugar swings and insulin resistance amplify inflammatory signalling through multiple pathways.
Chronic hyperglycaemia also increases glycation damage, further activating immune stress responses.
Explore: Insulin Resistance, Blood Sugar & Longevity and Glycation & AGEs.
8) Stress, cortisol and immune regulation
Chronic nervous system activation alters immune regulation and increases inflammatory tone.
Poor sleep, persistent anxiety and lack of recovery compound this effect over time.
See: Nervous System Ladder and Stress and Longevity.
9) How to reduce inflammaging safely
Move consistently
Regular movement improves immune regulation and reduces inflammatory baseline over time.
Protect sleep
Sleep is when inflammatory signalling resets.
Stabilise blood sugar
Metabolic stability lowers immune stress signalling.
Eat diverse whole foods
Fibre and polyphenols support gut and immune balance.
Manage stress load
Nervous system regulation lowers cortisol-driven immune dysregulation.
Suppression strategies (high-dose anti-inflammatories, chronic antioxidant megadoses) often backfire long-term.
FAQ
Is all inflammation bad?
No. Acute inflammation is essential for healing and immune defence.
Can I measure inflammaging?
Biomarkers exist, but trends and context matter more than single readings.
Do supplements reduce inflammaging?
Some may help selectively, but lifestyle foundations dominate long-term control.
How fast can inflammation improve?
Some markers improve within weeks of improved sleep, movement and diet — but structural resilience takes longer.
Final takeaway
Inflammaging reflects the cumulative stress placed on immune regulation over decades.
The most effective strategy is restoring recovery capacity, metabolic stability and nervous system balance — not suppressing inflammation blindly.
— Simon
References
- Franceschi C et al. (2000). Inflamm-aging: an evolutionary perspective on immunosenescence. Annals of the New York Academy of Sciences.
- Furman D et al. (2019). Chronic inflammation in the etiology of disease across the life span. Nature Medicine.
Simon is the creator of Longevity Simplified, where he breaks down complex science into simple, practical habits anyone can follow. He focuses on evidence-based approaches to movement, sleep, stress and nutrition to help people improve their healthspan.