The Gut–Immune Link: How Your Microbiome Shapes Inflammation, Ageing and Resilience
Your gut isn’t just about digestion. It trains your immune system, regulates inflammation, and shapes long-term health trajectories — making microbiome health a quiet driver of biological ageing.
← Back to: Biology of Ageing Explained
Disclaimer: This article is for educational purposes only and does not provide medical advice. It is not intended to diagnose, treat or prevent disease. Always consult a qualified professional before making major dietary or health changes.
Roughly 70% of your immune system sits in and around the gut. That alone should change how we think about digestion.
The gut isn’t just a food-processing tube — it’s an immune training ground, signalling hub, and regulatory interface between your external environment and internal biology.
When the gut ecosystem is balanced, immune responses stay precise, inflammation resolves efficiently, and metabolic signalling remains stable. When the gut barrier and microbiome become disrupted, low-grade immune activation can quietly persist for years — accelerating inflammaging and immune ageing.
This guide explains how the gut–immune connection works, why it matters for ageing, and how to support it without chasing probiotic hype or extreme diets.
Personal observation: The biggest lesson for me was realising that gut health isn’t about perfection — it’s about consistency. Fibre intake, food diversity, stress load and sleep quality all quietly compound in the background.
1) The simple explanation
Your gut microbiome helps educate your immune system.
Friendly microbes produce metabolites that:
- strengthen the gut barrier
- regulate immune tolerance
- reduce unnecessary inflammation
- support metabolic stability
When this ecosystem becomes imbalanced, immune signalling can remain chronically activated — contributing to inflammaging and immune ageing.
2) What the gut–immune system actually does
The gut-associated lymphoid tissue (GALT) contains a massive portion of your immune cells.
Its jobs include:
- distinguishing harmless food and microbes from true threats
- training immune tolerance
- preventing excessive inflammatory responses
- coordinating barrier repair
A healthy gut teaches the immune system restraint as much as defence.
3) How the microbiome trains immune function
Gut microbes ferment fibre and polyphenols into short-chain fatty acids and other bioactive metabolites.
These compounds:
- strengthen tight junctions in the gut lining
- regulate regulatory T-cells
- reduce pro-inflammatory signalling
- support metabolic signalling stability
Related: Polyphenols Explained and Anti-Inflammatory Foods.
4) Gut barrier integrity and inflammation
The gut lining forms a selective barrier between the external environment and circulation.
When barrier integrity weakens, bacterial fragments and toxins can enter circulation, triggering immune activation.
This doesn’t necessarily cause acute illness — but it can quietly raise baseline inflammatory tone.
5) Metabolic endotoxemia explained
Low-level leakage of bacterial endotoxins into the bloodstream is sometimes called metabolic endotoxemia.
This state is associated with:
- insulin resistance
- chronic inflammation
- fatigue and metabolic instability
Explore: Insulin Resistance and Blood Sugar & Longevity.
6) Why gut–immune function declines with age
- reduced microbial diversity
- slower epithelial turnover
- immune regulation drift
- lower fibre intake over time
- higher medication burden
- chronic stress exposure
These changes contribute to rising inflammatory load with age.
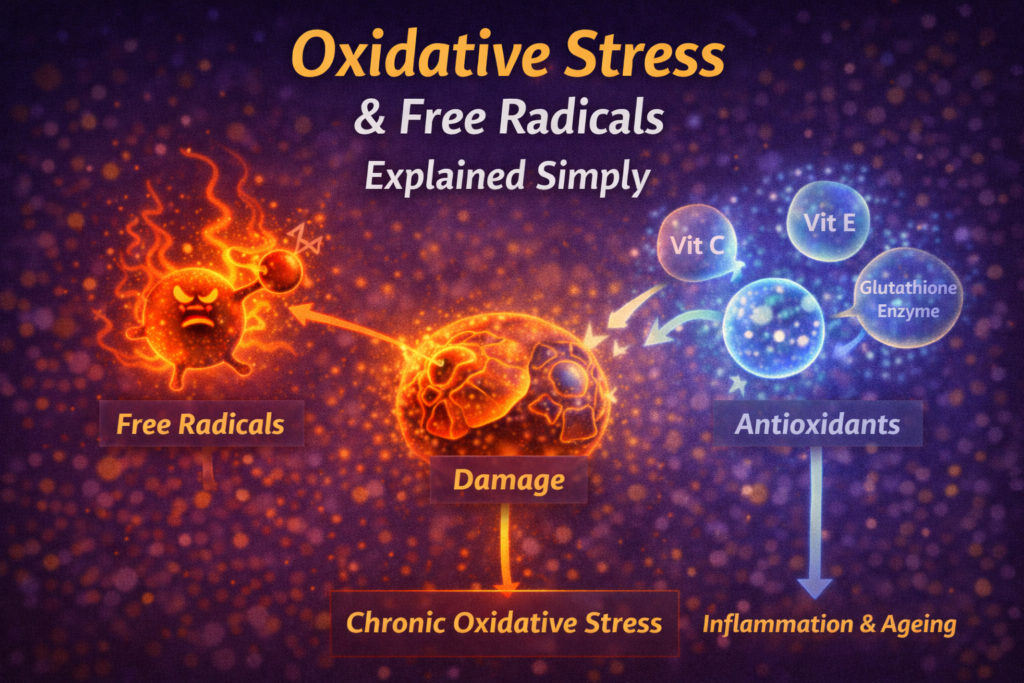
7) Oxidative stress, mitochondria and gut health
Oxidative stress and mitochondrial dysfunction can impair barrier repair and immune regulation.
Meanwhile, gut-derived inflammation increases systemic oxidative load — creating feedback loops.
Related: Inflammation vs Oxidative Stress, Mitochondria & Ageing.
8) Stress, sleep and gut signalling
The nervous system strongly influences gut motility, permeability and microbial balance.
Poor sleep and chronic stress can disrupt gut signalling and barrier integrity.
See: Nervous System Ladder and Sleep for Longevity.
9) How to support gut–immune health practically
Eat diverse plants regularly
Fibre diversity supports microbial diversity and metabolite production.
Include polyphenol-rich foods
Colourful plants feed beneficial microbial pathways.
Stabilise blood sugar
Large glucose swings stress gut and immune systems.
Protect sleep and recovery
Repair processes require adequate recovery.
Manage stress load
Nervous system regulation stabilises gut signalling.
Supplements may help selectively, but food and lifestyle dominate long-term outcomes.
FAQ
Do I need probiotics?
Not usually. Fibre diversity matters more for most people.
Is “leaky gut” always pathological?
No. Mild permeability shifts occur naturally. Chronic elevation is the concern.
Can gut health affect mood and stress?
Yes — gut–brain signalling is bidirectional.
How fast can gut health improve?
Microbial changes can occur within days, but stable improvements require consistency.
Final takeaway
Your gut shapes immune regulation, inflammatory tone and long-term resilience.
Simple daily behaviours — fibre diversity, stable meals, sleep and stress regulation — quietly compound into healthier ageing.
— Simon
References
- Belkaid Y, Hand TW. (2014). Role of the microbiota in immunity and inflammation. Cell.
- Cani PD et al. (2007). Metabolic endotoxemia initiates obesity and insulin resistance. Diabetes.
Simon is the creator of Longevity Simplified, where he breaks down complex science into simple, practical habits anyone can follow. He focuses on evidence-based approaches to movement, sleep, stress and nutrition to help people improve their healthspan.